Just before the sun began its slow descent below the horizon on April 22, 1915, thousands of German soldiers simultaneously twisted the knobs on metal cylinders containing chlorine gas. They released a rolling cloud that tumbled across “no man’s land” and into the unprepared trenches of the British Expeditionary Force defending the line at Ypres, France. Thousands died. In this first use of modern chemical warfare, all the advantages lay with the attacker. The British had no gas masks, their physicians did not know how to treat gas-related casualties, and their hospital infrastructure was not equipped to handle the strain of thousands of new patients. While the German military offensive floundered, medically Ypres was a disaster for the British and French. Over the next three years, warring countries worked to develop multi-tiered responses to the threat of chemical weapons.
U.S. advances technology and treatment
Since the U.S. did not enter World War I until 1917, it benefitted from the lessons learned by the French and British. The U.S. Army Medical Department (AMEDD) created a Chemical Warfare Service (CWS) to develop protective equipment, which allowed its physicians to focus on treatment.1,2 The CWS created an array of technologies to protect soldiers. Initially forced to adopt British small-box respirators when early American gas masks proved ineffective, the U.S. invested in a massive research effort, eventually deploying the Kops-Tissot-Monroe mask that became standard issue. The U.S. ultimately produced more than 5 million gas masks.2-4
The Army also devised numerous detectors that variously alarmed, beeped, and changed color in the presence of poison gas.3,4 Although it was recognized that North American snails frantically waved their tentacles when exposed to gas, this technique did not prove to be a practical warning device.5
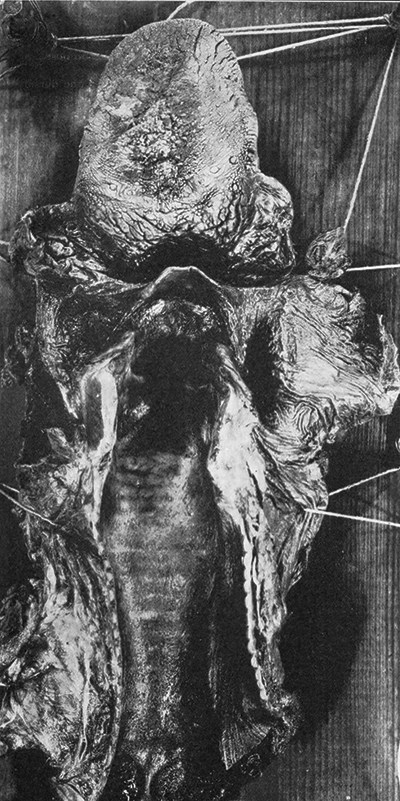
Once in Europe, AMEDD adopted the French “Z” system of evacuation, assigning one hospital per division to specialize in the care of chemical weapons victims (see Figure 1).1 AMEDD also deployed mobile decontamination units, which could cleanse 24 men every three minutes. When the men stripped to shower, medical officers examined their skin for evidence of gas exposure, triaging individuals who needed further care at specialized facilities (see Figure 2).3,5
Figure 1. AMEDD advance gas aid station