Editor’s note: This article is being posted electronically with the January Bulletin so that surgeons will have access to the important information it provides regarding changes in Medicare payment that took effect this month. Because of delays in the release of the final rule on the updates, this information was unavailable when the print version of the January Bulletin went to press, so the article will be published in the February 2021 print issue.
New payment policy, coding, and reimbursement changes set forth in the 2021 Medicare physician fee schedule (MPFS) final rule took effect January 1. The MPFS, which the Centers for Medicare & Medicaid Services (CMS) updates annually, lists payment rates for Medicare Part B services and introduces or modifies other regulations that affect physician reimbursement and quality measurement.
The American College of Surgeons (ACS) submitted comments September 22, 2020, in response to the CMS MPFS proposed rule issued earlier in the year.* Some provisions in the final rule, released December 1, 2020, incorporate the College’s recommendations. Although the final rule includes important payment and policy decisions that affect all physicians, this article focuses on updates that are particularly relevant to general surgery and its related specialties.
E/M office/outpatient visits
CMS did not make any changes to its reimbursement policies for office/outpatient evaluation and management (E/M) Current Procedural Terminology (CPT) codes 99202–99205 and 99211–99215 finalized in 2019 for calendar year (CY) 2021. Beginning January 1, 2021, CMS adopted the revised office/outpatient E/M code guidelines and descriptors created by the American Medical Association (AMA) Editorial Panel.† These new guidelines eliminate history and physical exam as elements for office/outpatient E/M code selection and allow physicians to choose the E/M visit level based on the extent of their medical decision making or total time spent on the day of the encounter.‡ For detailed guidance on reporting the new office and outpatient E/M codes, refer to the ACS Office/Outpatient E/M Coding Resource Center.
The agency also finalized an add-on code for office visits that are part of ongoing primary care and/or management of patients with serious or complex conditions. CMS had previously used “GPC1X” to refer to this office and outpatient E/M add-on code but finalized replacing GPC1X with Healthcare Common Procedural Coding System (HCPCS) code G2211. CMS affirmed that G2211 may be used for both new and established patient visits. The code descriptor for G2211 is, Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious condition or a complex condition. (Add-on code, list separately in addition to office/outpatient evaluation and management visit, new or established). CMS assumes that specialties that bill a majority of office and outpatient E/Ms will use G2211 for 90 percent of the office and outpatient E/Ms.
The ACS has continued to oppose the use of this add-on code and has strongly advocated, in both the regulatory and legislative arenas, for its withdrawal. Given the extensive changes to the office and outpatient E/M codes, G2211 is unnecessary because clinicians can simply bill a higher-level code for additional work, resources, or complexity. Following the publication of the final rule, Congress passed the Consolidated Appropriations Act of 2021, which suspended payments for G2211 for three years (through the end of December 2023). The legislation represents a significant win for surgeons by mitigating major budget neutrality cuts to Medicare physician payments for CY 2021.
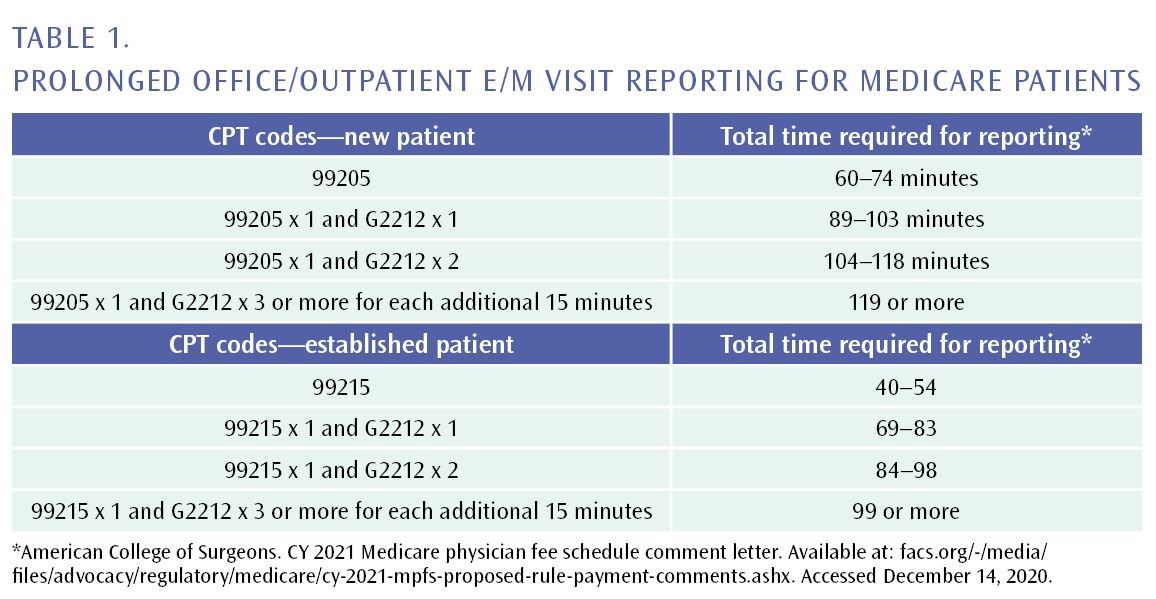
CMS also rejected the previously finalized CPT code 99417 for prolonged services and created new HCPCS code G2212 for Medicare patients. Private payors may continue to use 99417 and different rules apply for this code. When code selection is based on time (instead of MDM), code G2212 may be reported when the maximum time for the level 5 office/outpatient E/M visit is exceeded by at least 15 minutes on the date of service. Table 1 describes correct reporting of HCPCS code G2211.
When reporting based on time, the ACS also requested clarification that the total time that the reporting practitioner spent on the day of the visit (including face-to-face and non-face-to-face time) should be used when selecting office or other outpatient E/M level. The CPT guidelines could be interpreted as the total time of both a physician and a qualified health professional for code selection. The ACS commented that the most straightforward and auditable method for using time to select the level of an E/M service is to require that the time reflect the total time of the reporting practitioner. CMS agreed with this interpretation of the guidelines by stating in the final rule “the billing practitioner’s total time.”
CMS also finalized proposals that increased the values of certain codes because CMS stated that these codes are analogous to crosswalks to the office and outpatient E/M codes that increased in value, including codes for the following:
- End-Stage Renal Disease Monthly Capitation Payment Services
- Transitional Care Management Services
- Maternity Care Services
- Assessment and Care Planning for Patients with Cognitive Impairment
- Initial Preventive Physical Examination
- Initial and Subsequent Annual Wellness Visit
- Emergency Department Visits
- Physical and Occupational Therapy Evaluations
- Behavioral Health Services
The increased values of these codes are partially responsible for the reduction in the CY 2021 conversion factor because of the budget neutrality requirements for Medicare Part B payment.
Global codes
In 2019, CMS accepted the AMA Specialty Society Relative Value Scale Update Committee’s (RUC)-recommended work relative value units (RVUs) for office/other outpatient E/Ms for CY 2021, which will increase the RVUs for these services, but the agency will not apply the same incremental increases to postoperative E/M visits that are bundled into 10- and 90-day global codes.
The ACS commented extensively on this proposed policy, expressing strong opposition to CMS’ failure to apply increases to standalone office/outpatient E/Ms to global codes. The College’s comments stressed that this policy will disrupt the relativity of the MPFS because it will increase payment for certain specialties but not for others that provide the same services. CMS’ policy will pay different specialties different amounts for the same work, which is prohibited by law.
In addition, the agency ignored recommendations from nearly all medical specialties when this policy was discussed at the RUC, which voted overwhelmingly to recommend that the full increase of work and physician time for standalone office/outpatient E/Ms be included in global codes. The College opposes any policies that unfairly result in lower reimbursement for surgeons and will continue its advocacy efforts to contest CMS’ failure to increase values for the E/M portion of 10- and 90-day global codes.
Telehealth and other services involving communications technology
Through a series of interim final rules making various regulatory changes to the Medicare program in response to the COVID-19 pandemic, CMS revised, on an interim basis, coverage and reimbursement policies for telehealth and other virtual services during the national coronavirus (COVID-19) public health emergency (PHE). In the CY 2021 MPFS final rule, the agency made permanent several of these provisional telehealth-related requirements first introduced to reduce COVID-19 exposure risks.
Continued payment for audio-only visits
In March 2020, CMS established separate payment for audio-only telephone E/M services, which previously were considered non-covered under the MPFS, and increased the reimbursement rates for such services to match those of in-person established patient office/outpatient E/M codes.
CMS finalized a policy that stated audio-only E/Ms will no longer be separately payable by Medicare at the conclusion of the COVID-19 PHE, and instead will be assigned a “bundled” status. Consequently, the cost associated with providing audio-only E/Ms will be bundled into payment for other services to which they are incident.
Virtual presence of teaching physicians
CMS modified its teaching physician supervision and documentation policies during the PHE—and subsequently made such policies permanent in the CY 2021 MPFS final rule. Under the final rule, teaching physicians who meet CMS’ requirements may bill for services involving residents through interactive audio/video real-time communications technology, but only if the services are furnished by residents at training sites that are located outside of a designated metropolitan statistical area.
The agency clarified that when a teaching physician, through virtual presence, directly observes care rendered by a resident, the patient’s medical record must clearly reflect how and when the teaching physician was present for the service. For example, in the medical record, the teaching physician may document his or her physical or virtual presence at the training site during the key portion of a service, along with a notation describing the specific portion(s) of the service during which the teaching physician was present virtually.
In its comments on the proposed rule, the ACS opposed continued use of audio/video technology to provide direct supervision because of concerns about patient safety. For instance, in complex, high-risk, surgical, interventional, endoscopic, or anesthesia procedures, a patient’s health status can quickly change. The College stated that it is necessary for such services to be furnished or supervised in-person to allow for rapid on-site decision making in the event of an adverse clinical situation. A supervising physician may not be able to recognize or meet these urgent clinical needs through audio/video interactive communications technology as well as for other services provided concurrently. CMS acknowledged the ACS’ feedback and indicated that, for complex, high-risk procedures, the physical, in-person presence of the teaching physician is required during all key or critical portions of the procedure, and should be immediately available to furnish services during the entire service or procedure if necessary for patient safety given the risks associated with these services.
Electronic prescribing for controlled substances
The Substance Use Disorder Prevention that Promotes Opioid Recovery and Treatment (SUPPORT) for Patients and Communities Act of 2018 mandates electronic prescribing for controlled substances (EPCS) provided under Medicare Part D. In recognition of the time and resources practices must invest to comply with Drug Enforcement Agency guidance for EPCS, as well as additional challenges presented by the COVID-19 PHE, CMS delayed required practitioner compliance until January 1, 2022. The agency encourages prescribers to begin preparing for enforcement of EPCS requirements by integrating EPCS into their practices in 2021.
Conversion factor
In addition to delaying payments for G2211 until 2024, the Consolidated Appropriations Act of 2021 reduced the 10.2 percent cut to the CY 2021 conversion factor (CF) that was initially finalized by CMS in the MPFS to a 3.3 percent cut. Through this legislative change, the CY 2021 MPFS CF is now approximately $34.890—a $1.20 reduction—from the 2020 MPFS CF of $36.09. The 2021 CF reflects a statutory update factor and a budget-neutral adjustment as set forth in section 1848 of the Social Security Act (see Table 2).§
The Table 3 demonstrates the significant reduction in payment cuts for certain services commonly performed by general surgeons that were prevented in part because of the ACS’ advocacy efforts supporting the Consolidated Appropriations Act of 2021.