In 2016, both the adult colostomy and urostomy books were updated. Under the direction of Michael McGee, MD, FACS, a colorectal surgeon, and Jan Colwell, RN, MS, CWOCN, FAAN, representing the Wound, Ostomy, and Continence Nurses Society, new images and guidance on oral replacement fluids and dehydration management for ileostomy were added. The urostomy content, first developed under the guidance of Jack McAninch, MD, FACS, FRCS(Hon), a urological surgeon and recipient of the ACS Distinguished Service Award, was updated with other urinary diversion options. Content on long-term follow-up for the urostomy patient was conducted with guidance from two other urologists, Alexander Kutikov, MD, FACS, and Jay Raman, MD, FACS.
In 2018, all of the skills programs were integrated into the ACS Learning Management System to offer online training. Adult colostomy, adult urostomy (Spanish and English), and pediatric colostomy and pediatric urostomy are available via the ACS Ostomy Home Skills Program page.
The research portal for local studies also is completed, and sites can participate in quality improvement projects using the evaluation tools located in the ACS REDcap data collection platform.
An important feature of the skills training program is the collaboration between participating associations and the ACS Foundation. All the skills programs are partially supported by educational grants, with the Ostomy Kit funded by Coloplast since the kit’s inception. All ACS patient education skills kits follow the same Accreditation Council for Continuing Medical Education standards, including images of all common products, and are compliant with the U.S. Food and Drug Administration’s requirement that any product that is placed on the body include the manufacturer information.
Opportunities to participate in training programs
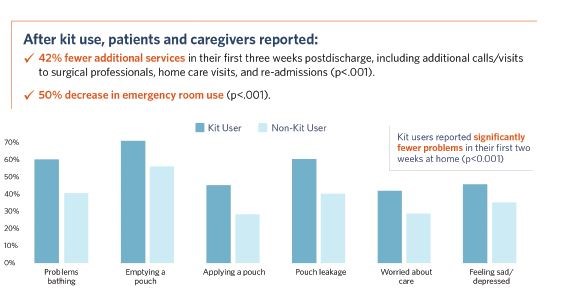
Ajit K. Sachdeva, MD, FACS, FRSCSC, FSACME, MAMSE, Director, ACS Division of Education, continues to emphasize the need to support the entire surgical community, including patients and caregivers, with the skills and education needed for the safe transition to home care. A standardized ostomy home skills kit that includes practice equipment, instruction delivered by a virtual coach, and checklists is an effective tool to support safe self-care postoperatively. The evidence-based program supports all members of the surgical team with an on-demand quality improvement application that increases confidence and satisfaction while reducing complications and expenditures.
Significant progress has been made with the introduction and validation of the patient and caregiver kit. Nonetheless, much more can be done to improve the quality of life for ostomy patients, in particular during the first 30 days after an operation, as they tend to the care of their new ostomy.
All patients have the opportunity to use the ostomy training program and can view the materials on the ACS website or sign up for the course in the ACS Learning Management System. Kathleen Heneghan, Assistant Director for Patient Education, ACS Division of Education, and coauthor of this article, said the most recent patient data indicate that patients who use the kit and practice with the pouches and ostomy simulator have the greatest confidence for self-care at discharge and have the highest degree of satisfaction.
The timing of the training also makes a difference. Patients who reported using the kit before surgery and then after discharge had better outcomes than patients first introduced to the training while in the hospital after surgery. These trends were seen for colostomy, ileostomy, and urostomy patients. A takeaway for all surgeons is to have the ostomy home skills kit available during the preoperative visit and instruct the patient and their caregivers to review the materials and practice. The instruction can then be reinforced in the hospital and at discharge using the skills kit checklist.
Education and training aimed at professionals and opportunities for sites to participate in controlled trials need to be completed to further improve how to best prepare a patient needing an ostomy. Does the skills validation or visits with a support group make a difference? Or are there other variables—such as body shape and contour, the way the pouch is applied in the operating room, and skin irritation at discharge from the health care facility—that affect the degree of complications?
Hospital and clinical sites also can participate in the registry-based ostomy education trial using the electronic evaluation tools. Participation in the trial will help determine the education methods that optimize outcomes for the ostomate. For access to the series of home skills programs and the ostomy program, visit www.facs.org/ostomy. For questions regarding the trial, contact Kheneghan@facs.org.
References
- Agency for Health Care Research and Quality. July 2020. Surgeries in hospital-based ambulatory surgery and hospital inpatient settings, 2014. Available at: www.hcup-us.ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.jsp. Accessed January 26, 2021.
- Weiss ME, Piacentine LB, Lokken L, et al. Perceived readiness for hospital discharge in adult medical-surgical patients. Clin Nurse Spec. 2007;21(1):31-42.
- Devine E, Cook T. Clinical and cost-saving effects of psychoeducational interventions with surgical patient: A meta-analysis. Res Nurs Health. 1986;9(2):89-105.
- Stenberg U, Vågan A, Flink M, et al. Health economic evaluations of patient education interventions: A scoping review of the literature. Patient Educ Couns. 2018;101(6):1006-1035.
- Heneghan K, Sachdeva AK, McAninch JW. Surgical patient education: Transformation to a system that supports full patient participation. Bull Am Coll Surg. 2006;91(6):11-19.
- Butler D. Early postoperative complications following ostomy surgery: A review. J Wound Ostomy Continence Nurs. 2009;36(5):513-519.
- Krouse R, Grant M, Ferrell B, Dean G, Nelson R, Chu D. Quality of life outcomes in 599 cancer and non-cancer patients with colostomies. J Surg Res. 2007;138(1):79-87.
- Salvadalena G. Incidence of complications of the stoma and peristomal skin among individuals with colostomy, ileostomy, and urostomy: A systematic review. J Wound Ostomy Continence Nurs. 2008;35(6):596-607.
- Colwell JC, Gray M. Does preoperative teaching and stoma site marking affect surgical outcomes in patients undergoing ostomy surgery? J Wound Ostomy Continence Nurs. 2007;34(5):492-496.
- Anderson L, Krathwohl D, Airasian P, et al. A Taxonomy for Learning, Teaching, and Assessing: A Revision of Bloom’s Taxonomy of Educational Objectives. Pearson. New York City; 2000.
- Heneghan KC, Sachdeva AK, Davis E, Bailey HR. Surgical skills patient education program. J Cancer Educ. 2009;24(S1):72.